
The quest to make a global vaccine in 12 months
[ad_1]
 Getty Images
Getty ImagesThe global quest to find a vaccine for Covid-19 has so far tended to focus on the clinical research, but manufacture and distribution also need to be considered.
Vaccines by themselves do not save lives, but rather the immunisation process does. This highlights a challenge the world is facing right now. The process used to create a vaccine in a laboratory is different to the one used for bulk manufacturing by the pharmaceutical industry in order to immunise people.
We already manufacture billions of doses of vaccines every year, from the annual influenza jab to the combined measles, mumps and rubella (MMR) immunisation. The 2009 swine flu pandemic, which saw the death of hundreds of thousands of people, lead to approximately three billion doses of flu vaccines being produced and delivered within six months.
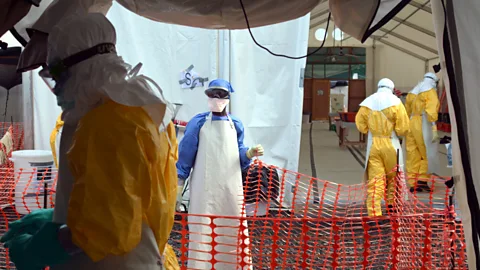
Developing a new vaccine is a lengthy process. The 2014 to 2016 Ebola outbreak in West Africa resulted in the death of more than 11,000 people. Scientists with the Public Health Agency of Canada had been working on the rVSV-ZEBOV vaccine since 2003 and it was only during the Ebola outbreak that the vaccine’s clinical trials were actually conducted. It was successfully concluded in November 2016 and was approved three years later following a further trial study with 15,000 people.
Creating and manufacturing an entirely new vaccine on a national or global scale, whilst maintaining production of all the other vaccines, becomes a Herculean endeavour, experts say. “We’re making a vaccine for a virus that we’ve never made a vaccine for, that’s not approved, using platforms that haven’t been used extensively in the clinic with patients,” explains Angela Rasmussen, a virologist at Columbia University’s Center for Infection and Immunity.
Conventionally, vaccine research can take 10 years from initial development through to mass distribution. However, for Covid-19, there is a global effort to reduce that to only 18 months, whilst maintaining the same safety standards.
Central to this is the parallel development process that the pharmaceutical industry is using during the crisis. Vaccine research is usually performed in a sequence of successive steps. Typically, there would be a laboratory development stage, followed by animal testing, and then several stages of clinical trials. Once these stages have been successfully completed, the vaccine would be submitted for approval, prior to developing a manufacturing process.
For Covid-19 vaccines, several stages of development are being carried out in parallel. This is necessary due to the urgent need for the vaccine, but it has the drawback that one stage of the process does not inform the next in the usual way. For example, results from animal trials would normally inform the choice of appropriate dose level for the start of human trials. The present situation is that data from several various stages are being analysed concurrently.
“We’re actually seeing preclinical data in non-human primates for vaccines that are already in phase three clinical trials,” explains Margaret Liu, chair of the board of the International Society for Vaccines.
 Getty Images
Getty ImagesAs part of the parallel development process, manufacturing facilities are already being built around the world, ahead of any vaccine being approved. This carries a significant financial risk, as there is a chance that certain vaccines may not be approved. It is only through enormous financial investment, such as $10bn (£7.85bn) for Operation Warp Speed, a US government initiative, that these facilities can be built in advance.
To bulk manufacture a vaccine, it is not a simple case of scaling up the process used in a laboratory. This is because it is analogous to baking a cake: if a recipe worked well for a small cake, tripling the ingredients may result in a cake that is burnt at the edges yet soggy in the middle. Similar issues are found in bulk vaccine manufacturing. “Processes that work well at a small scale in a test tube or petri dish often don’t behave in a predictable way in larger quantities,” explains Bryan Deane, director of new medicines and data policy at the Association of the British Pharmaceutical Industry.
A gradual up-scaling of the manufacturing process is therefore required. The vaccine will be manufactured in increasingly larger batches, with each batch checked to ensure efficacy is maintained. “There’s quite a lot of trial and error to achieve the best yield,” says Deane. “It takes time to work through those challenges of scale-up, until you get to a point where you’re getting a decent return on each batch that you put through.”
This problem is compounded by the fact that not all vaccine technologies, especially those that are showing the most promising results in clinical trials against Covid-19, have been used at such a large scale before. “Everyone is going to share the challenge of the large quantities that they’re trying to do,” explains Liu. “No vaccines have been utilised at this pace and scale for roll-out and the most advanced types of vaccine candidates have never been approved as vaccines at all.”
 Getty Images
Getty ImagesIn addition to this, many of the vaccines being developed require two doses in order to be effective, essentially doubling the number of vaccine doses required globally to nearly 16 billion. Only having a single shot of a vaccine, which requires multiple doses to be effective, can lead to problems.
“If people have low levels of antibody, but they think they’ve been immunised, one of the biggest risks is that then they will stop the social distancing and wearing masks,” says Liu. “Then they’ll get infected more easily, which in turn would make them capable of spreading the virus to others.”
Some vaccines also require special devices to be used. There are some DNA-based vaccines in development that require an electroporation device for each dose. Electroporation has previously been used to deliver a cancer drug into tumours. It uses a device the size of an electric toothbrush to generate a small electrical current that opens holes in the membrane of a cell, allowing a drug or vaccine to enter. Although the device can be used multiple times, it is nonetheless an additional manufacturing challenge in order to ensure there are a sufficient number of these. Medical staff would also need to have the appropriate training in how these devices are used.
And the supply of another piece of vaccine paraphernalia may also be an issue. Vaccines are generally supplied inside small glass vials. While it may seem surprising that glass is a limited resource, the glass used in vaccine vials is of a special type called borosilicate. It is highly resistant to temperature change and has low chemical reactivity, thereby minimising potential contamination from the vial. Given the colossal demand Covid-19 is generating for additional vials, this may constrain the number of vaccines that are initially available.
Multi-dosage vaccine vials might mitigate this problem, but could also lead to wasted doses if not all of the vaccine is used by the end of the day. When demand is at a premium, this sort of wastage must be avoided.
Of course, just having the vaccines is one thing, but keeping them safe and secure is another. Most vaccines need to be refrigerated, but some being developed for Covid-19 need to be stored in temperatures as low as -70°C (-94F) or -80°C (-112F). These kind of temperatures are commonly found in research laboratories, but many medical centres do not have such facilities.
In order to solve this cold storage problem, distribution companies such as UPS and DHL are building colossal freezer farms around the world, capable of storing millions of vaccines at -80°C (-112F), in order to have the appropriate facilities in place for when the vaccine is distributed.
 Getty Images
Getty Images“People have developed vaccine vial monitors, to make sure that the whole time there’s a recording of the temperature,” says Liu. “You don’t want something thawed and then refreeze it. You have to know what happens every second of the way during the transportation.”
There is also what is known as the Last Mile Problem. Distribution to major cities is fairly easy, due to them having transport hubs. However, getting it to smaller towns and remote villages, especially in developing countries, will be much more difficult.
By spring 2021 we could well see a gradual release of a vaccine for Covid-19 for priority cases, leading up to mass-distribution by the summer. In anticipation of this, steps are already being taken to ensure the manufacturing – and distribution – infrastructure is in place to meet the global demand.
This challenge may seem colossal, but what has already been achieved, through collaboration and working together like never before, demonstrates that it is not insurmountable.
[ad_2]
Source link





